
Is hospital management of self-harm improving?
The NICE guidelines on short and longer term management of self-harm were published in 2004 and 2011. They had an impact on care that people who self-harm receive in the emergency department.
In a study carried out by Cooper et al (2013), hospital management of self-harm in a national sample of general hospitals in 2010-2011 was compared with management at the same hospitals during 2001-2002. The chart below shows some of the key results from the study.
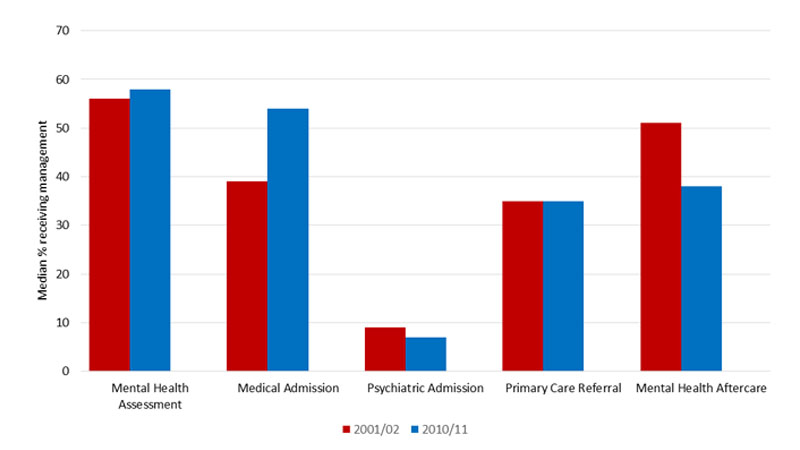
Although very little had changed in terms of practical management, such as the percentage getting a psychosocial assessment or psychiatric admission, this study also made an assessment of overall service quality in the hospitals via interviews with clinical staff at each site.
In assessments of service quality for people who attended the emergency department after self-harm, there were increases in quality in 75% of the hospitals included in the study.
It is recognised that there are challenges to implementing NICE guidelines, and NICE have taken steps to improve implementation of guidelines via publication of Quality Standards.
There is some evidence that bespoke training and eLearning resources on management of self-harm have a positive impact on helping to implement guidelines in clinical practice (de Beurs et al., 2015), and work to improve the implementation is on-going.
Psychosocial assessment
Our research suggests that psychosocial assessment following hospital presentation for self-harm could reduce the risk of repetition by 40% (Kapur et al, 2013).
But in 31 hospitals investigated, only just over half of patients received an assessment, though guidelines state this should be 100% (Cooper et al, 2013).
Alcohol use
Alcohol misuse and alcohol at the time of self-harm is associated with an increased risk of death by suicide, but people who are intoxicated are less likely to receive a psychosocial assessment (Ness et al, 2015).
A thorough psychosocial assessment may help with early identification of alcohol problems and help to identify appropriate interventions (Bergen et al, 2014).
Contacting general practitioners
Information regarding assessment is sent to GPs following only 36% of episodes, even though national guidelines state that this should be 100% (Cooper et al, 2013).
The breadth and depth of information sent to GPs was found to be poor, particularly from ED staff (Bergen et al, 2014).
