Support for improving community-based care for self-harm
The National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) is working alongside experts from the Manchester Self-Harm Project and the Patient Safety Translational Research Centre to support NHS Integrated Care Systems across England to improve community-based services and care for people who self-harm.
This is part of a national programme of transformation funded by NHS England and NHS Improvement linked to establishing new and integrated models of primary and community mental health care across England. These new models will provide improved care for adults and older adults who self-harm in the community, as laid out in the NHS Long Term Plan.
This work is commissioned by the Healthcare Quality Improvement Partnership (HQIP), with funding from NHS England and NHS Improvement.
We will support teams in participating areas by:
- providing broad expert knowledge of current self-harm data and research;
- providing guidance on national guidelines and recommendations for the care of people who self-harm;
- advising on methods of data collection to monitor and evaluate the impact of service changes for people who self-harm;
- developing an online resource to gather useful information in an easily accessible format.
Introduction to Community Based Care for Self-Harm – YouTube links and presentation slides
Please click through the following links to access recordings of Professor Nav Kapur introducing the Community Based Care for Self-Harm project, the work being done at some of the sites we are working with, and the support available from our team.
Phase I Virtual Site Visits
Nav Kapur on Improving Community Based Care
- Frimley Presentation
- Frimley Surrey Presentation
- Herefordshire Presentation
- Hertfordshire Presentation
- Humber Presentation
- Lincolnshire Presentation
- NE London Presentation
- NW London Presentation
- Sheffield Presentation
- Somerset Presentation
- S Yorkshire and Bassetlaw Presentation
Phase II Virtual Site Visits
22 February 2022
Community Based Care Virtual Site Visit (Full event)
23 February 2022
Community Based Care Virtual Site Visit (Full event)
26 April 2022
Community Based Care Virtual Site Visit (Full event)
- Nav Kapur Presentation
- Lancashire and South Cumbria Presentation
- Bristol South, Somerset and North Gloucestershire Presentation
- Lancashire and South Cumbria Ambulance Service Presentation
1 June 2022
Community Based Care Virtual Site Visit
8 June 2022
Community Based Care Virtual Site Visit
Phase II Virtual Clinics
- 31 March 2022 – Leah Quinlivan and Elizabeth Monaghan on Patient Involvement
- 31 March 2022 – Battle Scars Presentation
- 28 April 2022 – Dr Caroline Clements on Clinical Coding of Self Harm and Outcome Measurement
- 26th May 2022 – Dr Faraz Mughal, School of Medicine, Keele University
- 26th May 2022 Virtual Clinic – The Samaritans
- 23rd June 2022 – Dr Leah Quinlivan: Self-harm and safety plans
- 23rd June 2022 – Dr Emma Nielson: Adapting Safety Plans With and For Autistic Adults and Those Who Support Them
- 23rd June 2022 – Dr Claire Iveson: Collaborative Safety Planning Intervention
- 28 July 2022 – Cathy Morgan: Self Harm in older adults How Common How Managed And what re the outcomes
- 28 July 2022 – Dr Ali Baird: Self-harm in Older People ‘Don’t Brush it Under the Carpet’
- 28 July 2022 – Dr Amanda Thompsell: Self Harm and Older adults – Dispelling the myths
- 28 July 2022 – Harriet Bickley Self-harm in Older Adults Infographic, 28 July 2022
- 29 September 2022 – Laura Pisaneschi: One example of crisis follow-up, A&E follow-up clinic
- 29 September 2022 – Jonathan Haggerty & Dr Vish Goel, Evolution of self-harm follow-up in Sunderland PLY
- 29 September 2022 – Prof Nav Kapur: The new NICE self-harm guidelines, aftercare and intervention
- 27 October 2022 -Busra Ozen Dursun – Self-Harm and Suicide Prevention in South Asian Communities in the UK
- 27 October 2022 -Dr Caroline Clements – Self-Harm among ethnic minority children and adolescents
- 27 October 2022 Javed Rehman – involving peope from diverse communities in research and practice development (the hard-to-reach paradigm)
- 24 November 2022 – Dr Hazel Marzetti Homophobia, biphobia, trasphobia and beyond enhancing understandings LGBTQ+ suicide and suicide prevention
- 24 November 2022 – Dr Brendan J Dunlop Bisexuality and NSSI Explorations and next steps
Infographics
As part of this work we co-created infographics that reflect the main themes of the community self-harm and CQUIN (psychosocial assessments) interventions developed during the project. These infographics are intended to promote and share learning; they summarise the projects’ aims, project details, and outcome measures.
Data Dictionary
We have developed a data dictionary (PDF) providing a selection of process measures that can be used to help assess change as areas implement new strategies for supporting people who self-harm.
Resources: evidence and guidance around self-harm
The following sections contain links to information on different aspects of care for people who self-harm, such as national clinical guidelines, peer reviewed journal publications, and commissioned reports.
Section 1: guidance on assessment care and potential treatments
Clinical guidelines on care for people who self-harm
The following clinical guidelines draw together evidence for the best ways to provide care for people who self-harm.
NICE has produced clinical guidance on both the short- and long-term management of self-harm, as well as quality standards for the care of people who self-harm:
- Self-harm in over 8s: long-term management (2011)
- Self-harm in over 8s: short-term management and prevention of recurrence (2004)
- Self-harm quality standard (2013)
- New self-harm guidance from NICE is currently being finalised with publication expected in July 2022
NCISH developed a self-harm toolkit intended to be used as a basis for self-assessment by mental health care providers has been developed by NCISH and is available as a PDF online:
CQUIN
CQUIN stands for Commissioning for Quality and Innovation. This is a system introduced in 2009 to make a proportion of healthcare providers’ income conditional on demonstrating improvements in quality and innovation in specified areas of care.
Provision of good quality psychosocial assessments for patients who have self-harmed is a core clinical priority area. NHS England and NHS Improvement implemented a CQUIN indicator for psychosocial assessments for patients who are referred to liaison psychiatry services for self-harm in April 2021. The CQUIN goal is that 80% of patients referred to mental health liaison teams receive a psychosocial assessment concordant with the NICE guidelines for self-harm. The following documents provide more information, guidance, and CQUIN audit tool. For further information, please see https://future.nhs.uk/MHCQUIN/groupHome
Psychosocial assessments
In this section you will find guidance on psychosocial assessments. Psychosocial assessments are typically carried out by clinical staff and take into account many psychological and social factors to determine the care and support needs of people who self-harm:
- Does Clinical management improve outcomes following self-harm? Results from the Multicentre Study of Self-Harm in England (2013)
- Psychological assessment following self-harm: results from the multi-centre monitoring of self-harm project. (2008)
- Psychosocial assessment and repetition of self-harm: The significance of single and multiple repeat episode analyses (2010)
- Psychosocial Assessment of Self-Harm Patients and Risk of Repeat Presentation: An Instrumental Variable Analysis Using Time of Hospital Presentation (2016)
- Are hospital services for self-harm getting better? An observational study examining management, service provision and temporal trends in England (2013)
- Routine hospital management of self-harm and risk of further self-harm: propensity score analysis using record-based cohort data (2017)
- ‘Wasn’t offered one, too poorly to ask for one’ – Reasons why some patients do not receive a psychosocial assessment following self-harm: Qualitative patient and carer survey (2021)
- ‘Relieved to be seen’-patient and carer experiences of psychosocial assessment in the emergency department following self-harm: qualitative analysis of 102 free-text survey responses (2021)
Guidance on psychological and medical treatment for people who self-harm
The following works present information on the effectiveness of psychological and medical treatments for people who self-harm (including adults, children and adolescents):
- Psychosocial interventions following self-harm in adults: a systematic review and meta-analysis (2016)
- Pharmacological interventions for self-harm in adults (2015)
- Interventions for self-harm in children and adolescents (2015)
- Effective psychological and psychosocial approaches to reduce repetition of self-harm: a systematic review, meta-analysis and meta-regression (2016)
Safety Planning
- Safety planning-type interventions for suicide prevention: meta-analysis. (2021)
- The Effectiveness of the Safety Planning Intervention for Adults Experiencing Suicide-Related Distress: A Systematic Review (2021)
- Safety Planning Intervention: A Brief Intervention to Mitigate Suicide Risk (2012)
- Self-harm and suicide in adults: will safety plans keep people safe after self-harm (2021)
Risk assessments and risk scales
Research on the use of risk scales for predicting future risk in people who present to hospital for self-harm:
- Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data (2018)
- Predictive accuracy of risk scales following self-harm: Multicentre, prospective cohort study (2018)
- Which are the most useful scales for predicting repeat self-harm? A systematic review evaluating risk scales using measures of diagnostic accuracy (2015)
- Predicting suicidal behaviours using clinical instruments: Systematic review and meta-analysis of positive predictive values for risk scales (2018)
- Predicting suicide following self-harm: systematic review of risk factors and risk scale (2018)
- Risk assessment scales to predict risk of hospital treated repeat self-harm: A cost-effectiveness modelling analysis (2019)
- Suicide risk assessment in UK mental health services: a national mixed-methods study (2020)
- Accuracy of individual and combined risk-scale items in the prediction of repetition of self-harm: multicentre prospective cohort study (2020)
- Which are the most useful scales for predicting repeat self-harm? A systematic review evaluating risk scales using measures of diagnostic accuracy (2015)
- The assessment of clinical risk in mental health services (2018)
- Quality of risk assessment prior to suicide and homicide: a pilot study (2013)
Section 2: Services for self-harm and patient experience
Research assessing services for self-harm
Guidance on the current state of services available for people who self-harm in England:
- Pushed from pillar to post: Improving the availability and quality of support after self-harm in England (2020)
- Inquiry into the support available for young people who self-harm: A report by the All-Party Parliamentary Group on Suicide and Self-Harm Prevention
Papers:
Clinician and service user views on self-harm/mental health care
Clinician and service user views on self-harm/mental health care:
- Service user perspectives on psychosocial assessment following self-harm and its impact on further help-seeking: A qualitative study (2013)
- Learning from clinicians’ views of good quality practice in mental healthcare services in the context of suicide prevention: a qualitative study (2019)
- Patients’ experiences of emergency hospital care following self-harm: systematic review and thematic synthesis of qualitative research (2020)
- “Well it’s like someone at the other end cares about you.” A qualitative study exploring the views of users and providers of care of contact-based interventions following self-harm (2011)
- Needs and fears of young people presenting at accident and emergency department following an act of self-harm: secondary analysis of qualitative data (2018)
- Role of primary care in supporting older adults who self-harm: a qualitative study in England (2019)
- Role of the GP in the management of patients with self-harm behaviour: a systematic review (2020)
- Liaison psychiatry practitioners’ views on accessing aftercare and psychological therapies for patients who present to hospital following self-harm: Multi-site interview study (2023)
- Accessing psychological therapies following self-harm: qualitative survey of patient experiences and views on improving practice (2023)
Section 3: Improving awareness and training.
Promoting awareness of self-harm
People who self-harm often report poor staff attitudes when they seek help, which may discourage people from seeking help in the future during times of crisis.
Guidance on competencies for healthcare and other staff working with people who self-harm. The competencies are for working with children and young people (from 8 years upwards), adults and older adults (from 18 years upwards), and the public (community and public health):
- NHS Health Education England. Self-harm and Suicide Prevention Competence Framework
- Service user perspectives on psychosocial assessment following self-harm and its impact on further help-seeking: A qualitative study (2013)
- Learning from clinicians’ views of good quality practice in mental healthcare services in the context of suicide prevention: a qualitative study (2019)
- Role of the GP in the management of patients with self-harm behaviour: a systematic review (2020)
Staff training for self-harm
There are a number of free and paid training courses that might be helpful in raising awareness of self-harm among staff, dispelling myths and misconceptions about people who self-harm and promote improved care.
Free online training on the management and care of people who self-harm who attend the emergency department, with background information on self-harm and examples of patient experiences of care:
Training packages
- STORM provides bespoke training packages for suicide prevention and self-harm mitigation.
- Harmless provides support, information, and training about self-harm to people who self-harm, their friends, families and professionals, promoting health and recovery by increasing awareness and skill in intervention.
Although not self-harm specific, some organisations provide training courses focused on suicide prevention which include elements that may also be relevant to self-harm.
Section 4: Research on self-harm.
Statistics about people who self-harm
How have rates of self-harm changed over time and who is most likely to self-harm?
- Epidemiology and trends in non-fatal self-harm in three centres in England, 2000–2012: findings from the Multicentre Study of Self-harm in England (2015)
- Incidence and general hospital costs of self-harm across England: estimates based on the Multicentre Study of Self-Harm (2020)
- Suicide and self-harm in Britain: researching risk and resilience (2019)
- Prevalence of non-suicidal self-harm and service contact in England, 2000–14: repeated cross-sectional surveys of the general population (2019)
Characteristics of self-harm by age-group
-
Children and young people
- Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): a retrospective study (2018)
- Incidence, clinical management, and mortality risk following self-harm among children and adolescents: cohort study in primary care (2017)
- Self-harm in children and adolescents by ethnic group: an observational cohort study from the Multicentre Study of Self-Harm in England (2021)
- Self-harm in children 12 years and younger: characteristics and outcomes based on the Multicentre Study of Self-harm in England (2021)
- Mortality in children and adolescents following presentation to hospital after non-fatal self-harm in the Multicentre Study of Self-harm: a prospective observational cohort study (2020)
-
Adults (including people in midlife)
-
Older people
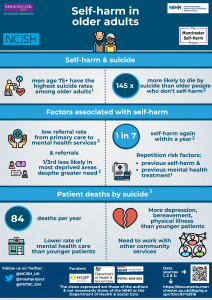
Self-harm in older adults
This infographic summarises published statistics about self-harm in older adults. It uses data from three sources: the Multi-centre Study for Self-Harm in England, the National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) and the NIHR Greater Manchester Patient Safety Translational Research Centre (NIHR GM PSTRC)/UK Clinical Practice Research Datalink (UK CPRD).
|
Self-harm in older adults infographic |
Self-harm in older adults data sources |
The Greater Manchester Suicide Prevention & Bereavement Support Programme campaigns to improve older people’s mental health: https://shiningalightonsuicide.org.uk/olderpeople/
Suicide and mortality following self-harm
People who self-harm are at much higher risk of going on to die by suicide compared to people in the general population:
- Suicide following presentation to hospital for non-fatal self-harm in the Multicentre Study of Self-harm: a long-term follow-up study (2019)
- Suicide and all-cause mortality following routine hospital management of self-harm: Propensity score analysis using multicentre cohort data (2018)
- Alcohol use and misuse, self-harm and subsequent mortality: an epidemiological and longitudinal study from the Multicentre Study of Self-Harm in England (2015)
Self Harm in primary care
- Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. (2017)
- Self-harm in a primary care cohort of older people: incidence, clinical management, and risk of suicide and other causes of death. (2018)
- The epidemiology of self-harm in a UK-wide primary care patient cohort, 2001–2013.
- South Asian women, psychological distress and self‐harm: lessons for primary care trusts. (2002)
- Premature death among primary care patients with a history of self-harm. (2017)
Self-harm and COVID-19
Early evidence of the impact of COVID-19 and associated health management measures (eg national and local lockdowns) on self-harm and mental health:
- The early impact of COVID-19 on mental health and community physical health services and their patients’ mortality in Cambridgeshire and Peterborough, UK (2020)
- Mental health and wellbeing during the COVID-19 pandemic: longitudinal analysis of adults in the UK COVID-19 Mental Health & Wellbeing study (2020)
- Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic (2020)
- Effects of the COVID-19 pandemic on self-harm. (2020)
- The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: a living systematic review. (2020)
- Self-harm during the early period of the COVID-19 pandemic in England: comparative trend analysis of hospital presentations. (2021)
- Characteristics and risk of repeat suicidal ideation and self-harm in patients who present to emergency departments with suicidal ideation or self-harm: A prospective cohort study. (2020)
- How to prevent, assess and manage the risk of suicide/self-harm during the COVID-19 pandemic. (2021)
- Digital – COVID-19 guidance for clinicians. (2020)
Section 5: Patient and public involvement
Patient involvement/ co-design
Helpful links on patient involvement and co-design. Some of these links are about research, but will be useful for quality improvement projects.
UK Standards for Public Involvement
National Institute of Healthcare Research (NIHR) helpful websites
NHS England Involvement Hub
HQIP Patient and public involvement in quality improvement
National Institute for Health and Care Excellence (NICE)
Section 6 : additional information
Brochures and pamphlets
Third sector organisations (selected, national)
Harmless: National service for self-harm; Email: info@harmless.co.uk; Phone: 01158800280
Self-Injury Support; Email: tessmail@selfinjurysupport.org.uk; Helpline: 0808 800 8088; Office/ Admin number; 0117 927 9600; Text support: 07537 432444
Battlescars, survivor led charity for people who self-harm: Email: info@battle-scars-self-harm.org.uk; Phone: 0741 0380747
Papyrus– for people under 35; Various contact details
Life Signs, Self-Injury Guidance & Support Network; Email: hello@lifesigns.org.uk
Rethink mental Illness; Phone: 0121 522 7007
SANE: Email: sanemail@sane.org.uk
People working on the project
We would like to thank all the staff and expert advisors who are working with us on this project.
Expert Reference Panel
We would like to particularly thank our Expert Reference Panel who have helped guide the development and implementation of this project. They are:
- Mette Isaksen – Samaritans, Lead for self-harm research
- Emily Cannon – Quality Improvement Coach, National Collaborating Centre for Mental Health
- Raili Frost – Senior project manager, NHS England
- Karen Lascelles – Nurse Consultant Oxford Health NHS Foundation Trust
- Caroline Harroe – CEO Harmless
- Ketan Sonigra – Clinical lead intensive case management, Principal Forensic Psychologist, South London and Maudsley NHS Foundation Trust (SLAM)
- Faraz Mughal – Academic GP, NIHR Doctoral Fellow, Keele University
- Declan Meehan – Clinical/operational Manager, Greater Manchester Mental Health Foundation Trust
- Amanda Thompsell – Consultant older age psychiatrist, Royal College of Psychiatrists
- Javed Rehman – Expert by experience, MS4MH-R
- Fiona Naylor – Expert by experience, MS4MH-R
- Stephen Barlow – Expert by experience, MS4MH-R
- Liz Monaghan – Expert by experience, MS4MH-R
Core Staff
Our core staff work at the University of Manchester in the Centre for Mental Health and Safety. They are:
- Professor Nav Kapur (Professor of Psychiatry and Population Health)
- Dr Pauline Turnbull (Project Manager/Research Fellow)
- Dr Leah Quinlivan (Research Fellow)
- Dr Caroline Clements (Project Manager/Research Fellow)
- Su-Gwan Tham (Research Associate)
- Iain Donaldson (Research Administrator)
- Bradley O’donovan (Research Administrator)