
Sector-specific evidence reports
The aim of this work package is to develop sector-specific evidence reports based on data, evidence and knowledge from PROTECT and elsewhere. For each sector, we present a summary of the evidence with links to relevant reports and papers for the details, and highlight the remaining evidence gaps with suggestions for further research.

Public transport
Overview
Public transport has been widely perceived as a high-risk sector for transmission of the COVID-19 virus, due to large numbers of people travelling in close proximity in enclosed spaces, often with limited ventilation. This report summarises the evidence currently available on COVID-19 infection and mortality among employees in the public transport sector, as well as risk factors for infection and infection control measures in this sector. We then highlight the remaining evidence gaps for each of these topics.
COVID-19 infection in the public transport sector
Evidence
- A literature review of studies up to May 2021 investigating transmission of SARS-CoV-2 (the virus that causes COVID-19) in public transport settings identified 28 papers assessing transmission, control measures or levels of contamination, with a focus on ground-based public transport.
- SARS-CoV-2 was detected in some surface and air samples in several studies, but detection of the virus did not necessarily indicate that the particles were still infectious.
- Three empirical studies from China early on in the pandemic provided evidence that proximity to an infected person and duration of travel in the same bus or train carriage as an infected person were important risk factors for COVID-19 infection.
- Overall, the review indicated limited evidence at the time on which to draw firm conclusions.
- Early results from surface sampling on public transport as part of the TRACK (Transport Risk Assessment for COVID Knowledge) study, combined with evidence from other studies, indicate that there is a low risk of transmission from contaminated surfaces, with airborne transmission the dominant route.
- The figure below shows estimates of the effect of working in the transport sector on risk of COVID-19 infection. In a Norwegian study bus and tram drivers were found to be at increased risk of infection in the first wave of the pandemic compared to other people of working age, but this relative risk reduced in the second wave, probably due to the introduction of preventive measures. Conductors and stewards had an increased risk compared to others of working age in the second wave but not the first, which may reflect greater numbers of passengers during the second wave. Changes in the criteria for COVID-19 testing between the first and second waves may have also affected the estimates.
- The UK Office for National Statistics (ONS) COVID-19 Infection Survey data show increased risk of infection for transport workers compared to non-essential workers, especially for taxi drivers and chauffeurs and bus and coach drivers (Rhodes 2021). The risk of severe COVID-19 infection was elevated in transport workers compared to non-essential workers in the UK Biobank cohort at the start of the pandemic.
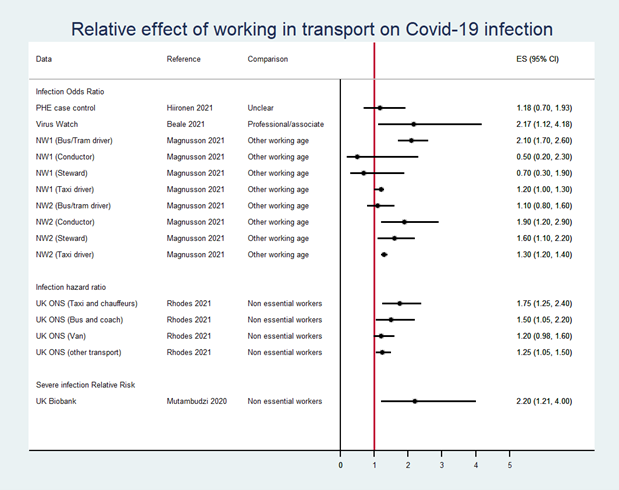
The figure shows an increased risk of COVID-19 infection among transport workers in some studies but not others. The details are provided in the text above.
ES: effect size. Greater than 1 indicates an increased risk, less than 1 indicates a decreased risk, e.g. an odds ratio of 2.17 (1.12, 4.18) indicates that transport workers had just over twice the risk of COVID-19 infection than professional/associate workers (and we can be 95% certain that the true effect size is between 12% more likely and nearly 318% more likely).
NW1/NW2: Norway wave 1/wave 2.
- Further analysis of Virus Watch data suggests that the risk of infection among transport workers in England and Wales, compared to professional/associate professional occupations, reduced in the third wave compared to the first two waves.
- It is important to be aware that differences in effect size estimates between the studies in the figure may in part be due to different methods and study designs. For example, the Norwegian study was a national study including the whole population whereas the Virus Watch analysis involved a sub-cohort of 3,761 participants in the UK Virus Watch prospective cohort study, who responded to monthly surveys.
- Virus Watch is one of the few datasets available to assess the risk of infection from using public transport (rather than working in public transport). Regular COVID-19 testing data and data on contact and activity patterns were collected from around 10,000 participants of the Virus Watch prospective cohort study during the second wave of the pandemic in England and Wales. Use of public or shared transport more than once per week was associated with 1.8 times increased odds of infection (adjusted odds ratio (OR) 1.82 [95% CI 1.49-2.23]), and was estimated to account for 12% of COVID-19 infections acquired outside the household (Hoskins et al. 2021).
- A qualitative study was conducted to understand perceptions of risk of SARS-CoV-2 transmission through interviews with experts, organisational leads, workers and passengers within the public transport sector (also see blog post). The risk of transmission on public transport was generally considered to be low. However, the interviews were carried out between January and May 2021 when passenger numbers were considerably reduced compared to pre-pandemic levels.
- Although most respondents thought transmission risk on public transport was low, rates were seen to vary and factors such as crowding, greater journey duration and non-compliance with mitigations were seen to increase risk.
- Some respondents felt that the government’s strong messaging on the risk of infection, and hence the need to avoid use of public transport unless essential, has had a lasting impact on passenger numbers.
Evidence gaps
- Further analyses are underway on how the risks for workers in the transport sector have varied over the different stages of the pandemic.
- Perceptions of risk of COVID-19 infection in the public transport sector may have changed since restrictions have been relaxed, with increasing passenger numbers and with vaccinations and new variants. Some of the respondents from the qualitative study are being interviewed again in January-March 2022 to assess this.
- It is important to improve our understanding of perceptions of risk among the general public, how these perceptions are changing, and how former passengers can be encouraged to use public transport again.
Workplace risk factors for COVID-19 infection
- Risk factors for COVID-19 infection which are particularly relevant for public transport settings are the inability to social distance in restricted spaces such as buses and train/tube carriages, and frequent contact with the general public.
- Age, deprivation, ethnicity, and region are non-workplace risk factors for COVID-19 infection and mortality, but some public transport workers are more likely to be in these risk groups. For example, some of the increased risk of death from COVID-19 among London bus drivers at the start of the pandemic can be (at least partly) explained by a high proportion of these workers being from vulnerable groups (older, from ethnic minorities and living in disadvantaged areas).
- These factors can be taken into account in analyses to understand the contribution of working in public transport to the risk of COVID-19 infection and mortality. For mortality, these other factors explain quite a lot of the increased risk in transport workers. However, adjusting for these factors does not substantially affect the estimates for risk of infection among transport workers.
- It is difficult to separate the impact of workplace risk factors from other factors which are strongly associated with occupation or direct consequences of work, such as shared accommodation and travel to work among co-workers and local/community levels of infection.
Evidence gaps
- Further work within the TRACK study is analysing CCTV data to further understand the impact of behaviour around social distancing, mask wearing and face touching on risks of transmission on public transport.
Workplace preventive measures to reduce COVID-19 infection
Evidence
- Evidence from studies investigating control measures in the public transport sector (identified in this literature review) indicates the importance of ventilation for reducing risk of SARS-CoV-2 (the virus that causes COVID-19) transmission, although the benefits of ventilation vary depending on the position of passengers in a bus and by the configuration of open windows in a taxi or car. There is evidence from simulation and modelling studies that face coverings also reduce the risk of transmission, although it is difficult to quantify the reduction in risk.
- In response to the high rates of COVID-19 deaths among London bus drivers early in the pandemic, the UCL VIRAL study made recommendations for modifications to the driver cab areas, based on analysis of air flow simulations. The existing perspex ‘assault’ screens were modified to minimise the gaps to reduce airflow between the passenger area and the driver cab area. A separate ventilation system was recommended for the driver cab area to minimise airflow from the passenger area, with the driver cab window open when possible.
- Modelling of transmission in a London underground carriage, as part of the TRACK study, showed that wearing face coverings reduces airborne and close-range droplet transmission (Miller et al. 2022).
- Recent evidence on the likely low risk of transmission from surfaces relative to risk from airborne aerosols and droplets may suggest that cleaning regimes could be modified with efforts focussed on effective ventilation systems. However, visible interventions such as cleanliness are associated with a perception of reduced risk and could increase passenger confidence in using public transport, so may be important to maintain.
- A qualitative study was conducted to understand perceptions of effectiveness of mitigation measures introduced in the public transport sector in the UK (as discussed in this blog post).
- Distancing, face coverings, additional cleaning, and hand sanitisation were introduced across the sector early on, with the importance of appropriate ventilation identified more recently. Work bubbles and staff testing have been implemented in some settings, although it was not always practical to set up workplace testing.
- Respondents reported good communication between companies within each sector, and preventive measures were usually introduced consistently across the public transport industry. There were some concerns around messaging for the public when changes to regulations were frequent and often differed between the devolved nations.
- Some respondents identified that it is difficult to know which measures are most effective, as most were implemented at speed and around the same time. However, in general, the measures were thought to be effective and frequently the low numbers of cases among employees were reported by respondents as evidence for this.
Evidence gaps
- More evidence is required on the relative effectiveness of different mitigation measures, to inform which should be continued or reinstated in future COVID-19 waves or new epidemics.
COVID-19 mortality in the public transport sector
- Analyses of routine mortality data from 2020 by occupation have shown that drivers and transport workers had some of the highest COVID-19 mortality rates among men.
- The Office for National Statistics (ONS) data for 9 March – 28 December 2020 on men aged 20 to 64 in England and Wales showed that the death rate among taxi and cab drivers and chauffeurs was 101.4 deaths per 100,000 males (209 deaths) and among bus and coach drivers was 70.3 deaths per 100,000 males (83 deaths). This compared to 31.4 deaths per 100,000 among all men aged 20 to 64. These rates were adjusted for age but not for other factors which may affect the risk of death from COVID-19.
- An analysis of mortality data for England linked to 2011 Census data (Nafilyan et al. 2021) showed that a large part of the differences in COVID-19 mortality between occupations could be explained by factors such as regional differences in COVID-19 prevalence, ethnicity, education, deprivation or pre-pandemic health.
- However, after adjustment for these other factors, among men, taxi drivers and van drivers were still at higher risk of death from COVID-19 compared to ‘non-essential’ workers* (see figure below). Taxi drivers were nearly 1.4 times more likely to die from COVID-19 than non-essential workers (fully adjusted hazard ratio 1.39 [95% Confidence Interval (CI) 1.14 – 1.70]). The fully adjusted hazard ratio for bus drivers was 1.11 [95% CI 0.85 – 1.45] and for van drivers was 1.26 [95% CI 1.03 – 1.55]. After full adjustment there was little evidence of an increased risk of mortality for other transport workers (e.g. train/tram drivers, large goods vehicle drivers, rail transport operatives, managers/directors in transport/distribution), who had a hazard ratio of 1.10 [95% CI 0.93 – 1.30]) compared to non-essential workers. Some of the differences in risk between categories of transport workers may depend on the level of contact with the general public.
- Increased mortality was also observed for women taxi drivers (see figure below). Note that the relatively low numbers of women in these occupations mean that the confidence intervals are wide.
* ‘Non-essential’ workers are those not in the following groups: healthcare workers, social and educational workers, other essential workers (including food, transport, police and protective services).
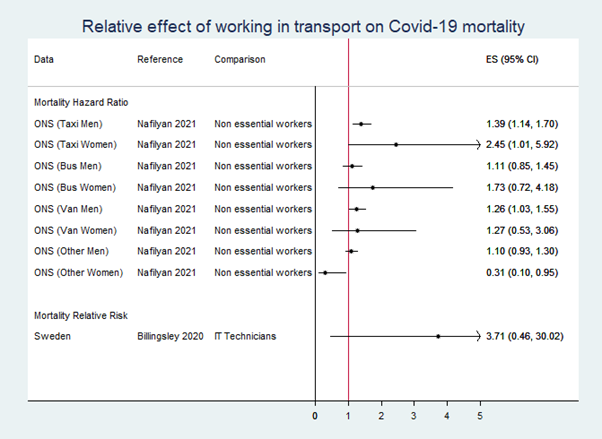
The figure shows an increased risk of COVID-19 death among some categories of transport workers but not others. The details are provided in the text above.
ES: effect size. Greater than 1 indicates an increased risk, less than 1 indicates a decreased risk, e.g. a hazard ratio of 2.45 (1.01, 5.92) indicates that women taxi drivers had nearly 2.5 times the risk of COVID-19 death than non-essential workers (and we can be 95% certain that the true effect size is between 1% more likely and nearly 500% more likely).
- To avoid issues related to inaccurate recording of cause of death, the impact of COVID-19 can be estimated by comparing death rates during the pandemic with rates before the pandemic, known as excess mortality. A study in California, USA, identified the highest per capita excess mortality (compared to pre-pandemic mortality Jan 2016-Feb 2020 among those aged 18-65) to be among transportation and logistics workers (91 per 100,000 [95% Prediction Interval (PI) 81-102]), a relative excess mortality of 31% (95% PI 26-36). This varied by ethnicity and was highest for Latino workers in this sector, at 47% (35-60), and lowest for white workers at 9% (4-15).
Evidence gaps
- Occupation data for the ONS analyses reported above was from the 2011 Census, and may therefore be out of date for some individuals. The 2021 Census data will soon be available for updated analyses. The analyses can also be updated to include COVID-19 deaths beyond the end of 2020, to investigate how the risk of death for transport workers has changed over time.
- There is evidence of differences in vaccine uptake by occupation (Nafilyan et al. 2021). Now that the vaccine programme is well-established in the UK, future analyses could assess the impact of these differences in uptake on mortality differences by occupation.

Food and drink processing sector
Overview
Food and drink processing facilities have the potential to be high risk settings for transmission of SARS-CoV-2 (the virus that causes COVID-19), as they are part of the critical infrastructure that remained open throughout the pandemic and often involve large numbers of workers in close proximity.
COVID-19 infection in the food processing sector
Evidence
- A literature review of 26 studies (Hosseini et al. 2022) identified reports of several outbreaks of COVID-19 infection in meat processing facilities in the USA early in the pandemic but there was limited evidence in UK settings.
- An analysis of Public Health England data for May – October 2020 (Chen et al. 2021) linked to workplace settings found the highest rate of COVID-19 infection outbreaks among manufacturers and packers of food (based on 117 outbreaks).
- In contrast, data from the Office for National Statistics (ONS) COVID-19 Infection Survey for April 2020 to October 2021 did not show a higher risk of COVID-19 infection among food production workers compared to non-essential workers (adjusted hazard ratio 0.88, 95% confidence interval 0.65 – 1.19) (Rhodes 2021). The risk in food production workers was lower than for other essential workers such as food retail and distribution, education and transport workers.
- Potential reasons for the inconsistent findings between these studies include:
- In the ONS Infection Survey analysis, the category of food production workers includes farming, agriculture and fishing (who tend to work outside and are therefore likely to have lower risks of infection) in addition to food process operatives and managers, who are likely to work in facilities involved in the manufacture and packing of food, as identified in the Chen et al. study.
- Migrant and temporary workers are unlikely to be included in the ONS Infection Survey but contribute a large proportion of the workforce in some food processing facilities.
- The figure below shows estimates of the effect of working in the food production sector on risk of COVID-19 infection. Although there was some evidence of an increased risk of COVID-19 infection for food preparation and hospitality workers compared to professional and associate workers in the Virus Watch cohort (Beale et al. 2021), this was not observed in the UK Biobank study.
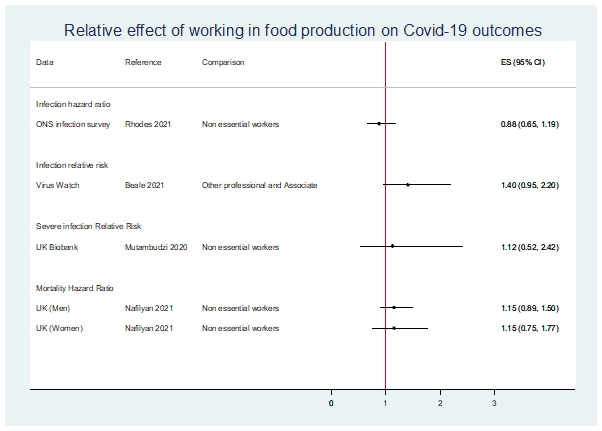
The figure shows estimates of the effect of working in food production on risk of COVID-19 infection and risk of death from COVID-19. The details are provided in the text above and in the section below.
ES: effect size. Greater than 1 indicates an increased risk, less than 1 indicates a decreased risk, e.g. an odds ratio of 1.40 (0.95, 2.20) indicates that food production workers had a 40% increased risk of COVID-19 infection than professional/associate workers. Note that the 95% confidence interval includes one; we can be 95% certain that the true effect size is between 5% less likely and 120% more likely.
Evidence gaps
- Further work is needed to understand the relative contributions of exposure to SARS-CoV-2 (the virus that causes COVID-19) in the workplace and in work-related settings such as shared accommodation and shared transport to work.
COVID-19 mortality among food processing sector workers
Evidence
- There was no evidence of an increased risk of death from COVID-19 among food production workers compared to non-essential workers in an analysis of mortality data for England linked to 2011 Census data (Nafilyan et al. 2021) (see figure above).
Evidence gaps
- Occupation data for the ONS analyses reported above was from the 2011 Census and may therefore be out of date for some individuals. The 2021 Census data will soon be available for updated analyses.
- It is important to note that occupation may not be accurately recorded for migrant and temporary workers. This could affect the COVID-19 mortality estimates for the food industry, where a large proportion of the workforce in some sub-sectors are seasonal, temporary or migrant workers.
- Uptake of COVID-19 vaccination varies by occupation (Nafiylan et al. 2021). These differences may impact on rates of infection, COVID-19-related illness and risk of death in different occupations.
Workplace risk factors for COVID-19 infection in the food processing sector
Evidence
- The literature review of studies in the food processing sector (Hosseini et al. 2022) identified several factors associated with an increased risk of COVID-19 infection:
- Ethnicity: non-white ethnic groups were disproportionately affected in several US studies
- Environmental factors: there were increased risks in workplaces with colder and more humid environments and poor ventilation.
- The COVID-19 At Work baseline survey (Mueller et al. 2022) included responses from 33 food and drink processing companies representing 66 sites across the UK.
- Higher infection rates were associated with higher deprivation (based on the Index of Multiple Deprivation score of the local area), a lower proportion of remote workers, a lower proportion of workers in close proximity, and higher numbers of workers overall.
- A qualitative study (Stage 3 of the Covid at Work Study) was conducted to understand perceptions of risk of COVID-19 infection and challenges and enablers to successful mitigation measures across the food processing sector. 21 semi-structured interviews were conducted with 32 individuals representing the following stakeholder groups: government agency/departments, academics, federations/associations and unions.
- In general, respondents did not consider the risk in the food processing sector to be higher than other similar industries.
- Respondents identified the following risk factors for infection which are specific to the sector: reliance on manual labour rather than automation, which involves large numbers of workers in close proximity on production lines; cold ambient temperatures and humidity – difficult to maintain adequate ventilation with chilled air.
- It was acknowledged that the risk of COVID-19 infection varies between different sub-sectors of the food and drink processing industry. Sub-sectors considered to be at particular risk of outbreaks are meat processing, agricultural food picking/production and sandwich making.
Evidence gaps
- A better understanding of the role of temperature and ventilation in transmission of SARS-CoV-2 would help to mitigate risks in the food processing sector.
Workplace preventive measures to reduce COVID-19 infection in the food processing sector
Evidence
- Several of the studies summarised in the literature review (Hosseini et al. 2022) discussed preventive measures in food production facilities, including social distancing, enhanced cleaning and disinfecting of high-touch areas, enhancement of ventilation and providing more community and work-based testing.
- The COVID-19 At Work Stage 2 survey (Covid at Work Summary Report) of 24 sites followed up 6-9 months after the baseline survey showed that most sites had implemented most of the mitigation measures that were asked about. These included: physical barriers, floor markings, one-way systems, increased workplace cleaning, non-touch options, CO2 monitoring, temperature checks (visitors, staff), provision of PPE and mental health support.
- The most commonly cited mitigations by respondents in the qualitative study (Stage 3 of the Covid at Work Study) included cleaning and hygiene practices, social distancing, measures to limit contact (e.g., screens, one-way systems, cohorts, staggering shifts), ventilation, testing and monitoring (surfaces and workers), PPE/face masks. Most respondents reported good compliance with preventive measures although some commented that social distancing was difficult to maintain within and outside operational areas.
Evidence gaps
- More evidence is required on the relative effectiveness of different mitigation measures in different sub-sectors of the food and drink processing industry. A tailored approach in each setting is likely to be most cost-effective and sustainable for future COVID-19 waves.
