Systemic inflammation affects reperfusion following transient cerebral ischaemia.
Burrows, F., Haley, M., Scott, E., Coutts, G., Lawrence, C., Allan, S. & Schiessl, I. (2016) “Systemic Inflammation Affects Reperfusion Following Transient Cerebral Ischaemia.” Experimental Neurology. 277, p. 252-60 9 p.
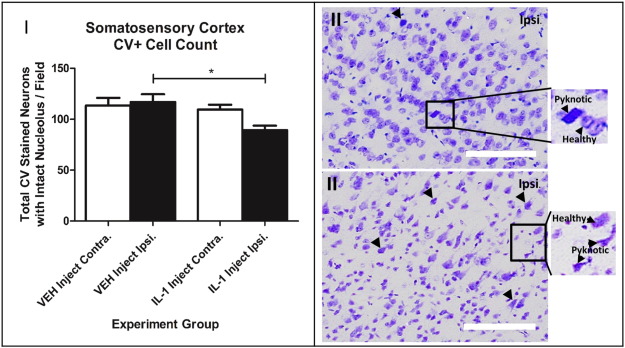
Reperfusion after stroke is critical for improved patient survival and recovery and can be achieved clinically through pharmacological (recombinant tissue plasminogen activator) or physical (endovascular intervention) means. Yet these approaches remain confined to a small percentage of stroke patients, often with incomplete reperfusion, and therefore there is an urgent need to learn more about the mechanisms underlying the no-reflow phenomenon that prevents restoration of adequate microvascular perfusion. Recent evidence suggests systemic inflammation as an important contributor to no-reflow and to further investigate this here we inject interleukin 1 (IL-1) i.p. 30 min prior to an ischaemic challenge using a remote filament to occlude the middle cerebral artery (MCA) in mice. Before, during and after the injection of IL-1 and occlusion we use two-dimensional optical imaging spectroscopy to record the spatial and temporal dynamics of oxyhaemoglobin concentration in the cortical areas supplied by the MCA. Our results reveal that systemic inflammation significantly reduces oxyhaemoglobin reperfusion as early as 3h after filament removal compared to vehicle injected animals. CD41 immunohistochemistry shows a significant increase of hyper-coagulated platelets within the microvessels in the stroked cortex of the IL-1 group compared to vehicle. We also observed an increase of pathophysiological biomarkers of ischaemic damage including elevated microglial activation co-localized with interleukin 1α (IL-1α), increased blood brain barrier breakdown as shown by IgG infiltration and increased pyknotic morphological changes of cresyl violet stained neurons. These data confirm systemic inflammation as an underlying cause of no-reflow in the post-ischaemic brain and that appropriate anti-inflammatory approaches could be beneficial in treating ischaemic stroke.
Read the full article here.






0 Comments