Diagnosis of food allergy
It is important to use reliable methods to diagnose food allergy in order to avoid unnecessary dietary restrictions. It is also important to understand that diagnosis of food allergy is generally not based on a single test.
Individuals with food allergy develop symptoms by eating foods that are simply part of a healthy diet for the vast majority of the population.
The only way for the allergic individual to manage their condition is to avoid eating the food that causes the allergic reaction.
Unfortunately, the public generally overestimates the number of people with food allergy. As a result many people avoid certain foods unnecessarily. Reliable diagnostic methods are required in order to avoid such unnecessary dietary restrictions.
 Accurate food allergy diagnosis is a specialised procedure requiring considerable clinical expertise. Currently, there are a range of diagnostic tests and procedures available to medical doctors.
Accurate food allergy diagnosis is a specialised procedure requiring considerable clinical expertise. Currently, there are a range of diagnostic tests and procedures available to medical doctors.
Diagnosis requires a compelling clinical history, positive skin prick test, positive allergen-specific serum immunoglubin E, and/or oral food challenge.
All the current diagnostic tests have advantages and shortcomings. Further research is required to develop more accurate, convenient, and cost-effective tests.
Self-diagnosis
Self-diagnosis of food allergy is notoriously unreliable, and failing to have a serious food allergy diagnosed could be potentially life-threatening. Therefore, people who suspect that they have a food allergy should seek specialist medical advice.
Currently, there are a range of diagnostic tests and procedures such as skin prick testing, blood tests, and challenge testing available to clinicians.
Diagnostic tests
 Generally, people with health problems first visit a primary care physician, such as a GP. In most European countries physicians refer patients to specialists when they suspect food allergy.
Generally, people with health problems first visit a primary care physician, such as a GP. In most European countries physicians refer patients to specialists when they suspect food allergy.
To diagnose food allergy the medical specialist will first take a full clinical history, and perform a clinical examination.
The clinical history will record details of past allergic reactions and other allergic conditions such as asthma, eczema and hay fever, and consider any seasonal or environmental symptoms, as well as any other relevant medical observations.
The clinical examination consists of a close look to see if there are allergic symptoms involving the skin, eyes and nose.
If the patient is asthmatic, the clinician may assess this by measuring the capacity of the lungs. This information will help the specialist decide which tests are appropriate.
The first test is usually a test for the detection of food-specific IgE antibodies, which have been shown to be predictive of IgE allergies, although they do not infer severity (Maloney, Rudengren et al. 2008).
A second test may be used, which is called a food challenge test.
Skin prick and blood tests
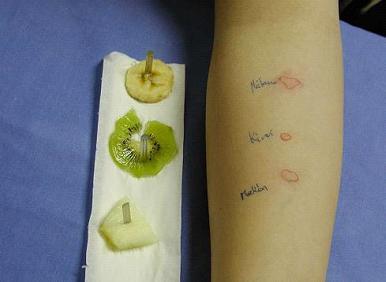
Skin prick tests are inexpensive, minimally invasive and results are immediately available.
In the skin prick test a tiny prick is made with a 1mm lancet through which drops of allergen extracts placed on the skin.
The test is positive if the skin becomes red and swollen at the site of allergen entry. A reaction of at least 3mm diameter is considered positive (Heinzerling, Mari et al, 2013).
In the blood test a blood sample from the patient is analysed for food-specific IgE antibodies using allergen extracts.
Generally, blood or skin prick tests used by medical specialists are efficient in ruling out allergy to a food when the test result is negative. However, in some cases the tests are negative, but a patient may still have symptoms when consuming a food.
The reliability of the results for example depends on the quality and stability of the food allergen extracts used. It is therefore important to use evaluated and well-documented tests and allergen extracts.
The presence of food-specific IgE (a positive test) does not necessarily mean that a person will experience symptoms of food allergy. The medical specialist will therefore interpret any test result in combination with findings from the clinical examination and the patient’s clinical history.
For that reason it remains the case that accurate food allergy diagnosis is a specialised procedure requiring considerable clinical expertise.
Food challenge test
A positive challenge test with a suspect food provides strong evidence of food allergy.
In a challenge test the patient eats a suspect food in gradually increasing amounts under controlled conditions to see if allergic symptoms occur.
Challenge tests are performed under supervision of allergy specialists in a hospital or clinic, where routines to safely manage any serious reactions are established.
For older children and adults, challenges are normally conducted in a double-blind manner with a placebo control. This is when neither the patient, nor the investigator knows whether or not the food preparation contains the specific allergen under investigation hidden in it.
A negative double-blind placebo controlled challenge test should be followed by an open challenge to avoid problems of false negative results.
Today double-blind placebo-controlled food challenges remain the “gold standard” in food allergy diagnosis, except where the patient has suffered anaphylaxis.
This is because both the skin prick tests and blood tests, although indicative, cannot directly predict allergy symptoms. The food challenge test is, however, not always performed as it is time consuming and more stressful for the patient than the other tests.
Even though this test is the gold standard in food allergy diagnosis, the test may produce false negative results, as it usually do not reproduce the circumstances under which the patient has experienced an adverse reaction.
The occurrence and severity of an allergic reaction may be influenced by for example exercise, what food is eaten at the same time, infections, stress, and intake of alcohol or medicine. The challenge test cannot detect delayed reactions occurring after the observation period.
Unproven diagnostic methods
Many websites advertise alternative diagnostic methods, e.g. measurement of food-specific IgG antibodies, hair analysis, cytotoxic tests, kinesiology, iridology and electrodermal testing.
The usefulness of these methods for food allergy diagnosis has not been proven by scientific studies. Therefore, clinicians and scientists cannot recommend the use of these methods in the diagnosis of food allergy.
These tests may also lead to false diagnoses of food allergies, resulting in unnecessary strict avoidance diets. At worst, these tests may wrongly indicate that someone with an allergy is not allergic to certain foods, which could cause them to eat a food they are allergic to and have a life-threatening reaction.
Further reading
Lay information:
- Pia Nørhede (2007) Food allergy diagnosis today and in the future
EuroPrevall state of the art paper:
- Asero, B.K. Ballmer-Weber, K. Beyer, A. Conti, R. Dubakiene, M. Fernandez-Rivas, K. Hoffmann-Sommergruber, J. Lidholm, T. Mustakov, J.N.G. Oude Elberink, R.S.H. Pumphrey, P.S. Skov, R. van Ree, B.J. Vlieg-Boerstra, R. Hiller, J.O. Hourihane, M. Kowalski, N.G. Papadopoulos, J.-M. Wal, E.N.C. Mills, Stefan Vieths (2007) IgE-Mediated food allergy diagnosis: Current status and new perspectives
Other papers:
- Sicherer, S. H., & Sampson, H. A. (2018) Food allergy: a review and update on epidemiology, pathogenesis, diagnosis, prevention, and management
- Turnbull, J. L., Adams, H. N., & Gorard, D. A. (2015) The diagnosis and management of food allergy and food intolerances
- Stapel SO, Asero R, Ballmer-Weber BK, Knol EF, Strobel S, Vieths S, Kleine-Tebbe J (2008) Testing for IgG4 against foods is not recommended as a diagnostic tool: EAACI Task Force Report
- Wüthrich B (2005) Unproven techniques in allergy diagnosis
