
Safer care for patients with personality disorder
Date of publication: February 2018
This report examined the characteristics of patients with a diagnosis of personality disorder prior to suicide or homicide. We wanted to learn more about their treatment and pathways into care, and whether services were adhering to NICE guidelines. We also asked patients and staff about their experiences of services, and how they thought services might be improved.
Key messages
Patients are not receiving care consistent with NICE guidelines
 Patients with personality disorder who died by suicide or committed homicide were not receiving care consistent with NICE guidance.
Patients with personality disorder who died by suicide or committed homicide were not receiving care consistent with NICE guidance.
NICE guidelines recommend that:
- patients should be offered appropriate and timely psychological interventions;
- medication should only be prescribed short-term;
- admission to in-patient care should be avoided where possible.
An examination of personality disorder services is needed
 There was no clear care pathway to meet the needs of patients with a diagnosis of personality disorder, and there was a lack of support and treatment for patients who did not meet the criteria for specialist services.
There was no clear care pathway to meet the needs of patients with a diagnosis of personality disorder, and there was a lack of support and treatment for patients who did not meet the criteria for specialist services.
We suggest a comprehensive examination of services for personality disorder is needed, taking into account the key recommendations from our report.
Working with patients to reduce stigma
 Although personality disorder is part of international classification systems, in practice, applying the diagnosis of personality disorder may be stigmatising and obscure individual needs. Working with patients to understand their traumatic experiences is likely to be more beneficial.
Although personality disorder is part of international classification systems, in practice, applying the diagnosis of personality disorder may be stigmatising and obscure individual needs. Working with patients to understand their traumatic experiences is likely to be more beneficial.
Safer prescribing
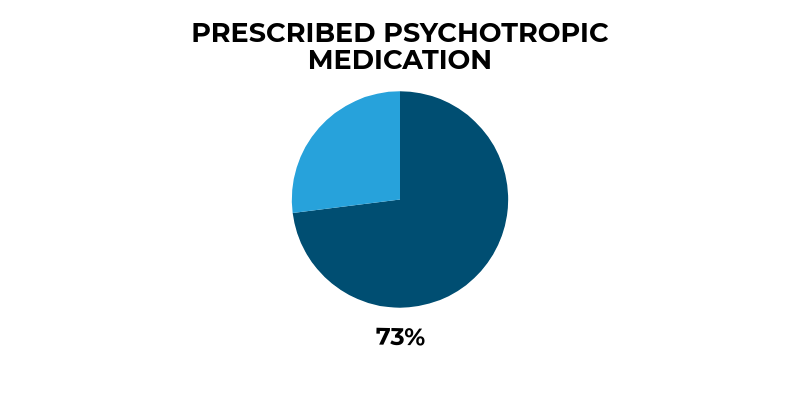
The majority of patients with a diagnosis of personality disorder had been prescribed psychotropic medication in the year before suicide or homicide (73%). This high number is of particular concern as the most common suicide method was self-poisoning, and antipsychotic medication was used in 20% of these deaths, antidepressants in 17%.
This emphasises the importance of safe prescribing in mental health services and primary care.
Substance misuse
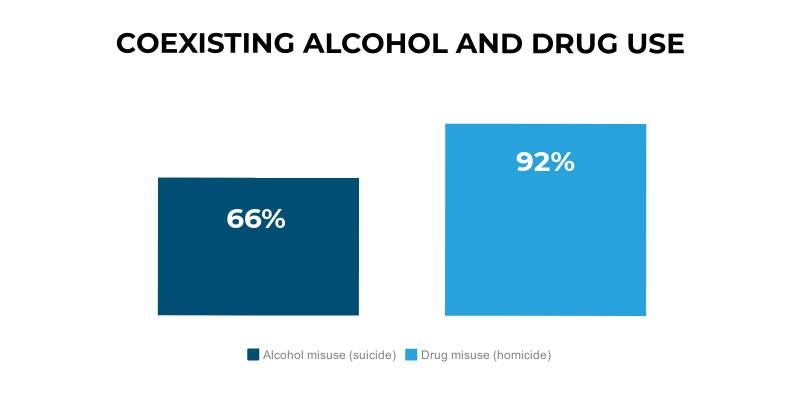
Risk in personality disorder is linked to co-existing drug and alcohol misuse. This shows the need for substance misuse services to be available.
Patient involvement in staff training, advocacy and peer support
 Former patients are an under-used resource and should have involvement in staff training, advocacy and peer support where possible.
Former patients are an under-used resource and should have involvement in staff training, advocacy and peer support where possible.
