
The assessment of clinical risk in mental health services
Date of publication: October 2018
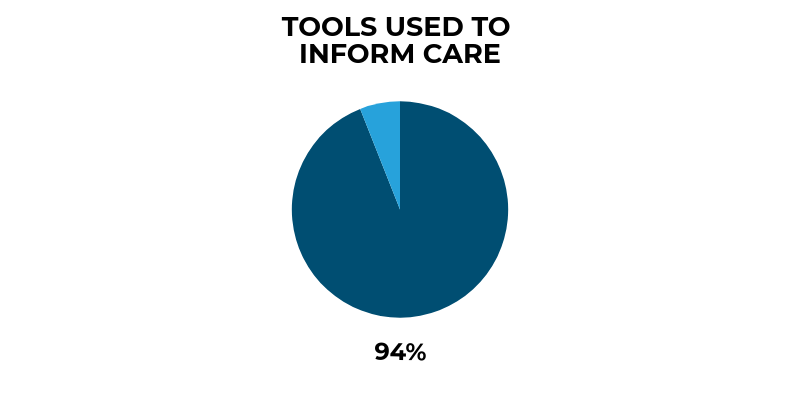
This study examined which risk assessment tools are currently used in mental health services. We wanted to identify how effectively these tools were being used prior to patient suicide, especially in patients rated as at low or no risk of suicide at their final contact with a mental health professional. We also asked staff, patients, and carers about their experience of risk and safety assessment, their views on the effectiveness of risk assessment tools, and how their use might be improved.
Key messages
Risk assessment tools should not focus on prediction
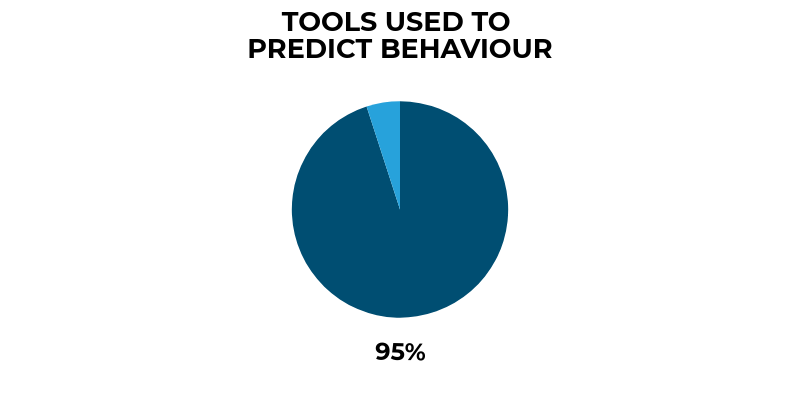
Most risk assessment tools sought to predict future behaviour. Risk assessment tools should not be seen as a way of predicting future suicidal behaviour.
Risk assessment is not a checklist
Risk is not a number, and risk assessment is not a checklist. Tools if they are used (for example as a prompt or a measure of change) need to be simple, accessible, and should be considered part of a wider assessment process. Treatment decisions should not be determined by a score.
Risk assessment is not a stand-alone or one-off process
 There is a growing consensus that risk tools and scales have little place on their own in the prevention of suicide. We suggest clinical risk assessment processes might be improved; by placing the emphasis on clinical judgement and building relationships, and by gathering good information on (i) the current situation, (ii) history of risk, and (iii) social factors to inform a collaboratively-developed management plan. Staff should be comfortable asking patients about suicidal thoughts.
There is a growing consensus that risk tools and scales have little place on their own in the prevention of suicide. We suggest clinical risk assessment processes might be improved; by placing the emphasis on clinical judgement and building relationships, and by gathering good information on (i) the current situation, (ii) history of risk, and (iii) social factors to inform a collaboratively-developed management plan. Staff should be comfortable asking patients about suicidal thoughts.
Staff training
 Risk assessment processes are an intrinsic part of mental health care but we suggest they need to be consistent across mental health services. Staff should be trained in how to assess, formulate, and manage risk. On-going supervision should be available to support consistency of approach. There is little place for locally developed tools.
Risk assessment processes are an intrinsic part of mental health care but we suggest they need to be consistent across mental health services. Staff should be trained in how to assess, formulate, and manage risk. On-going supervision should be available to support consistency of approach. There is little place for locally developed tools.
Family and carer involvement in the assessment process
 Families and carers should have as much involvement as possible in the assessment process, including the opportunity to express their views on potential risk. The management plan should be collaboratively developed where possible. The findings suggest consulting with the patient’s GP may also be helpful.
Families and carers should have as much involvement as possible in the assessment process, including the opportunity to express their views on potential risk. The management plan should be collaboratively developed where possible. The findings suggest consulting with the patient’s GP may also be helpful.
Personalised risk management
 The management of risk should be personalised. Risk assessment is one part of a whole system approach that should aim to strengthen the standards of care for everyone, ensuring that supervision, delegation and referral pathways are all managed safely.
The management of risk should be personalised. Risk assessment is one part of a whole system approach that should aim to strengthen the standards of care for everyone, ensuring that supervision, delegation and referral pathways are all managed safely.
